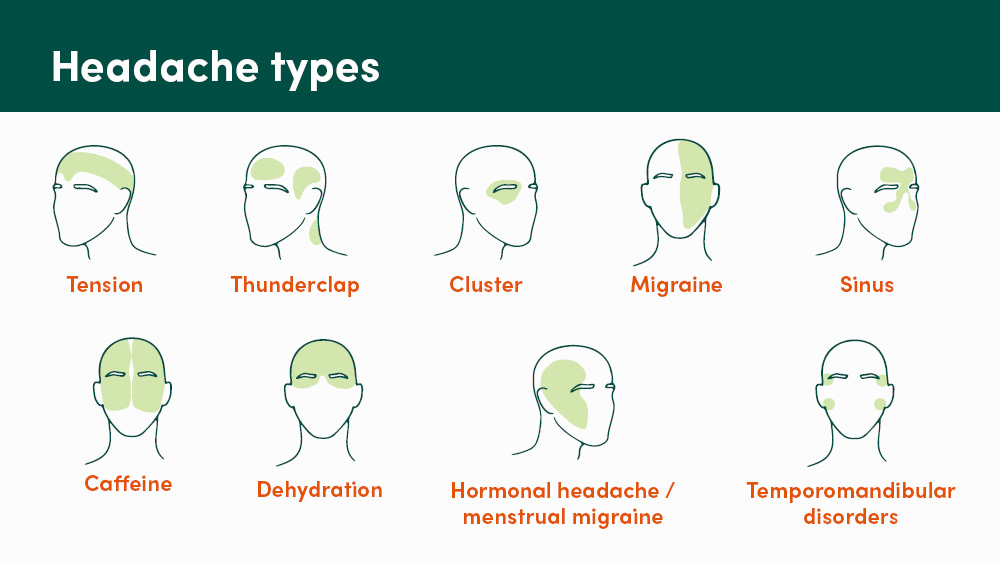
Experiencing a headache is painful. Have you ever wondered why your head hurts in certain locations? While it can be a minor inconvenience for some, it can be debilitating for others. Below are some common types of headaches and what they mean.
Types of headaches
While headaches can be common, they can vary widely depending on the causes and implications. Understanding the type of headache you’re experiencing is the first step in finding effective relief and preventing future occurrences.
-
Tension: sensation of mild to moderate tightness or pressure across the forehead, sides and/or back of the head
As the most common type of headache, tension headaches occur because of stress, lack of sleep, dehydration, eye strain, anxiety, poor posture or muscles strain. Sometimes, it can be described as feeling a ring around your head.
Normally, over-the-counter pain medications, such as acetaminophen, ibuprofen, aspirin or naproxen can help alleviate the pain. You may also consider lifestyle changes to reduce tension headaches.
-
Cluster: severe, piercing pain around one eye and/or temple
Cluster headaches are less common but are extremely painful and occur in cycles or clusters. In addition to feeling pain behind your eyes, you may also experience eye or face redness, as well as a runny or congested nose. The exact cause is unknown, but it’s believed to involve the hypothalamus – an area of the brain that controls hormones. Cluster headaches can be associated with obstructive sleep apnea, tobacco smoking, genetics and head trauma.
Acute treatment includes oxygen or a Triptan prescription. Patients with less frequent, bothersome attacks may benefit from a short course of steroids. Your provider could recommend the best medications based on your health history.
-
Migraines: throbbing pain, usually on one side of your head
Migraines are a genetic neurological disease that can significantly affect quality of life. It can be triggered by hormonal changes, certain foods, stress or environmental factors.
Those suffering from migraines are usually sensitive to their other senses. For example, light, movement, smells and sounds can make migraines worse. You may feel nauseous to the point of vomiting, and you may see zigzag or dots of light in your vision.
Over-the-counter medication can help, but if it doesn’t resolve, you can visit your primary care provider to review your treatment options, such as Botox® for migraines or other migraine-specific acute and preventative options.
You may also consider these lifestyle changes:
Hydration: In general, women should have at least 80 ounces of water daily and men should have at least 120 ounces of water daily. Of course, this can vary based on size, age and health conditions. Discuss what is best for you with your provider.
Diet: Eat at least a small snack every 3-4 hours while awake; this helps to stabilize blood sugars and keeps your brain and other body systems happier. Try to eat fresh food and cook at home. Processed foods often have added flavors, colors and preservatives that can be triggers for certain headache disorders.
Sleep: Keep a consistent and relaxing bedtime routine. Discuss sleep difficulties with your primary care provider.
Stress management: Practice mindfulness, meditation and/or prayer daily to help stress management, as well as sleep.
Medication use: If taking over-the-counter medication more than twice weekly, you could be at risk for developing rebound or medication overuse headaches. Talk with your primary care provider about dosing limits.
-
Sinus: pain behind your eyes, nose and/or cheekbones
If you have a sinus infection, cold or allergies, you can also experience a sinus headache. Often, the front of your face can be in pain.
Depending on your initial diagnosis, it can be resolved with antibiotics or a decongestant.
-
Thunderclap: severe, abrupt head pain
Thunderclap headaches can happen suddenly and last up to five minutes. You will feel intense pain.
It’s important to seek medical attention if you think you’re experiencing a thunderclap headache. The underlying cause could be serious, including vascular or blood vessel problems, injury or uncommon structural problems in the brain.
Some thunderclap headaches are not dangerous, but to be safe, seek medical attention if you’re experiencing sudden, severely painful headaches that disappear after a few minutes.
-
Temporomandibular disorders: pain in temples
Temporomandibular disorders (TMD) are multiple conditions that cause pain and dysfunction in the jaw joint and the muscles controlling jaw movement. Temporomandibular joints are located on each side of your face; it’s where your jaw meets your skull. This pain can trigger headaches.
By meeting with your primary care provider, you can learn about your treatment options, such as physical therapy or taking medications.
-
Hormonal headache/menstrual migraine: aching or pulsing head pain
Headaches can be triggered when estrogen levels change, which is what can happen during a menstrual cycle. Because every body is different, the location of the headache can change. Often, the forehead is the most common area you’ll feel pain with a headache during menstruation.
Over-the-counter medication can help, but if not, talk to your primary care provider to learn about other medications or therapies suitable for you.
-
Caffeine: aching or pulsing head pain
If you drink caffeine, your body begins to expect it and will react with a headache or migraine if it doesn’t receive its normal amount of caffeine.
To reduce your number of caffeine-induced headaches or migraines, you could keep track of how much caffeine you ingest a day to see if you can slowly reduce the amount, so your body isn’t dependent on it. Try to limit your caffeine intake to no more than 200 milligrams daily.
-
Dehydration: aching head pain, dizziness, extreme thirst
When you don’t drink enough water, your brain and tissues react by becoming smaller; this puts pressure on your nerves and causes pain.
Drinking the correct amount of water and resting will help resolve dehydration. If you feel extreme dizziness or pass out, it’s important to visit your nearest emergency room.
Discuss your symptoms with your primary care provider, who may refer you to a pain or headache specialist or a neurologist based on your symptoms. Contact your primary care provider to discuss your symptoms to see if you need a referral to a specialist.
This blog was medically reviewed by a MercyOne provider.